Dr. Nia Heard-Garris of Northwestern University undertook a comprehensive evaluation that found continuing healthcare inequities for racial and ethnic minority children compared to white children across pediatric disciplines. The Lancet Child & Adolescent Health’s two-part series on racism and child health illuminates disparities in neonatology, primary care, emergency medicine, inpatient and critical care, surgery, developmental disabilities, mental health, endocrinology, and palliative care.
Child Health Inequities: Urgent Pediatric Specialties Change Call
The neonatology part demonstrated that Black and Native American deficient birth weight infants received less human milk at hospital discharge.
In primary care, Black parents received fewer HPV vaccination recommendations for their children. The emergency department had the most considerable pediatric discrepancies in wait times, triage acuity, and child abuse examinations. Prescriptions for antidepressants to minorities were slower to decrease post-FDA warning.
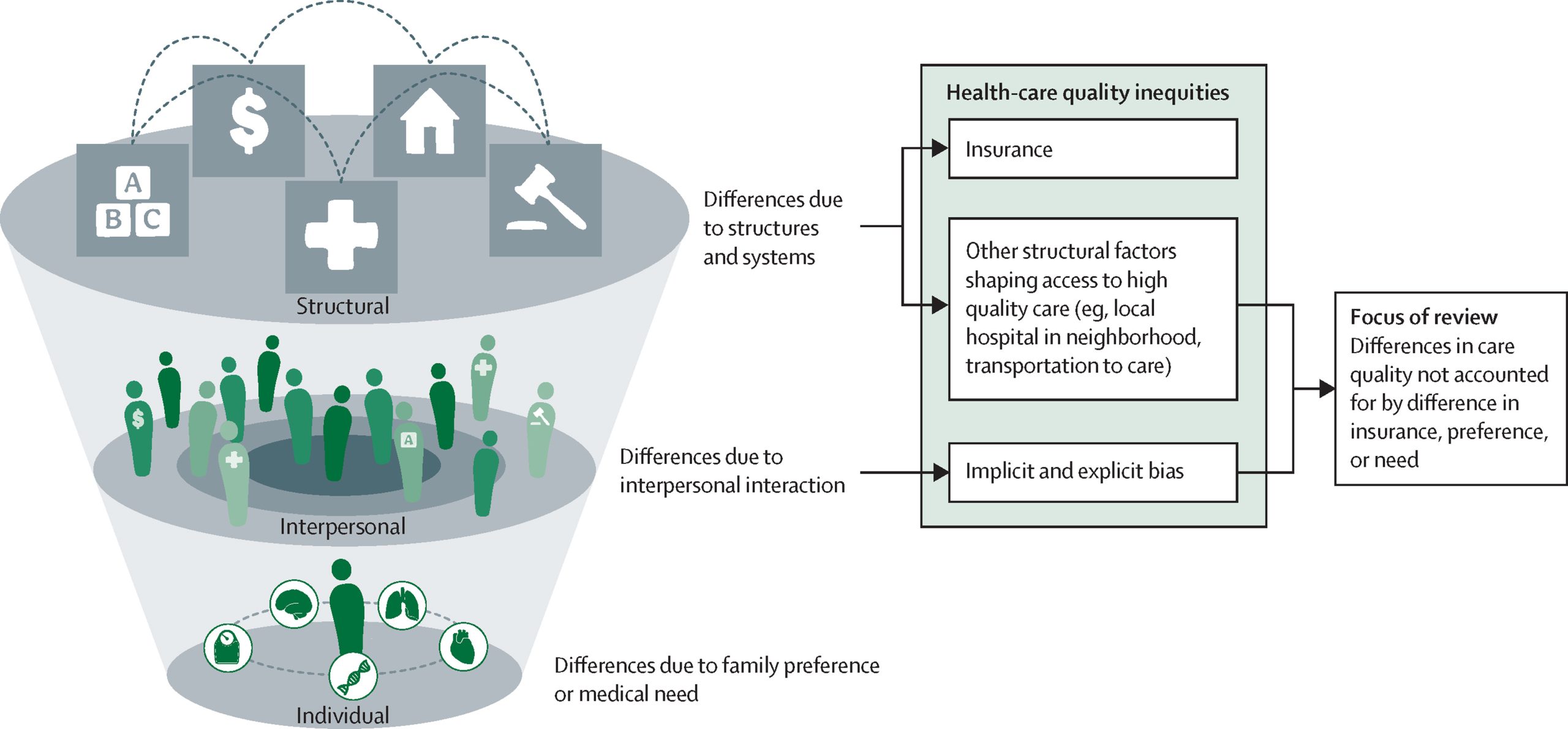
Implicit biases, prejudices, place of care, provider characteristics, and specialty training may have caused these discrepancies.
READ ALSO: Health agencies are on high alert due to measles outbreaks in the US and the UK
Urgent Calls for Change and Equity in Child Health
It suggests qualitative, quantitative, and mixed-methods research to identify and remediate inequitable treatment determinants. Equity measurements, repeated audits with provider feedback, reducing pediatric care racial segregation, and expanding medical workforce diversity are their recommendations.
A companion paper examined how housing, work, health insurance, immigration, and criminal justice policies affect child health equity. Community investment efforts, mortgage or rental help, federal minimum benefits for safety-net programs, expanded federal- and state-funded health insurance eligibility, and parental incarceration changes were recommended.