The global challenge of obesity has reached critical proportions, with approximately 1 billion individuals classified as obese in 2020 according to body mass index (BMI) standards.

Groundbreaking interventions termed “new obesity treatments” are taking center stage, offering innovative avenues for addressing this burgeoning public health crisis
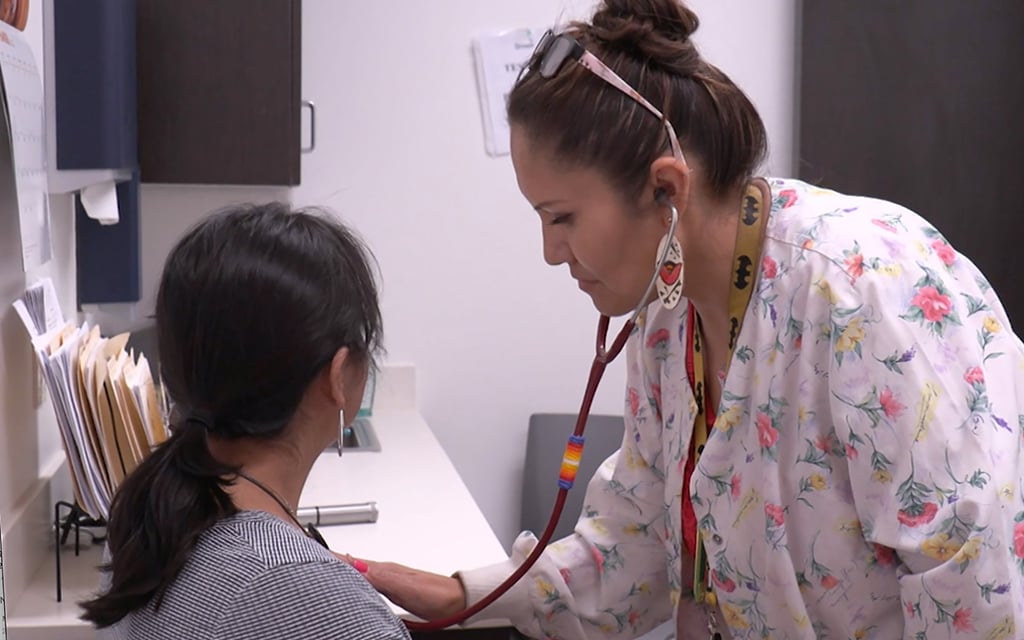
Obesity, a condition linked to a host of severe health issues including hypertension, diabetes, stroke, and various cancers, contributed to 5 million deaths in 2019 alone. Furthermore, the associated stigma often leads to mental health challenges such as depression, low self-esteem, and suicidal thoughts, further complicated by obstacles in accessing appropriate medical care due to weight-based discrimination. Although new obesity treatments advocate for calorie reduction and increased physical activity, the multifaceted nature of obesity often renders these approaches ineffective in the long term.
Recent times, however, have witnessed a paradigm shift, viewing obesity through a medical lens rather than a moral shortcoming. This transformation has sparked the development of new obesity treatments aimed at permanent weight loss. A notable breakthrough includes the emergence of “glucagon-like peptide-1 receptor (GLP-1) agonists,” a class of drugs mimicking the body’s natural hunger-suppressing hormone. Originally intended for diabetes management, these new obesity treatments have demonstrated substantial weight loss benefits, with clinical trials reporting participants shedding between 10-20% of their body weight. Promising contenders like Novo Nordisk’s Wegovy and Saxenda, alongside Eli Lilly’s Mounjaro, are already approved or projected to be approved as new obesity treatments.
Despite these new obesity treatments, achieving a tangible impact on the obesity epidemic hinges on accessibility
GLP-1 agonists, currently costing approximately $1,000 monthly, often lack insurance coverage due to their classification as “lifestyle” rather than medical necessities. A potential breakthrough lies in Novo Nordisk’s study revealing a 20% reduction in heart disease-related risks among GLP-1 users, which could encourage expanded coverage by insurers and Medicare.
The quest for solutions extends beyond pharmaceuticals, with researchers exploring brain stimulation techniques. Electrode implantation trials have shown promise in controlling hunger-related brain regions. Similarly, gene editing techniques hold the potential for permanently altering fat metabolism, with early studies in mice yielding encouraging results.
While the new obesity treatment landscape evolves rapidly, equitable access remains a core challenge. Alongside scientific advancements, transforming societal perceptions about obesity and reducing discrimination are pivotal to ensuring holistic success in combating this global health crisis.
READ ALSO: Innovative Local Job Fair Sets New Standard By Air-Dropping Barbecue For Attendees