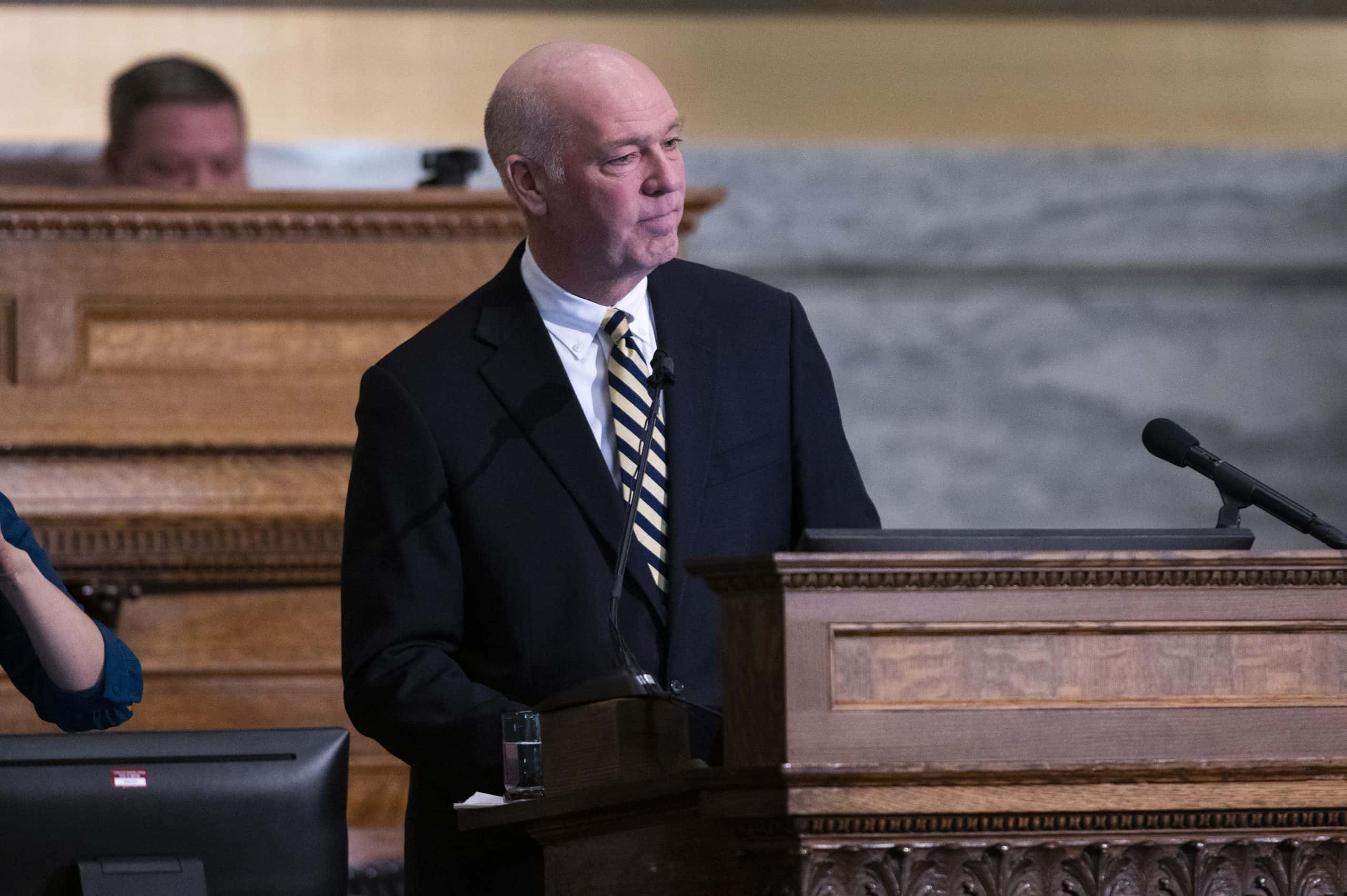
Montana Governor Greg Gianforte has signed the state’s primary budget bill, amounting to approximately $14.3 billion, which sets the financial roadmap for the next two years.
The budget includes significant increases in reimbursement rates for healthcare providers who serve Medicaid patients
The governor’s office highlighted several key aspects of House Bill 2, such as tax cuts, investments in state infrastructure, support for affordable childcare and housing programs, and a substantial boost to Medicaid provider rates, which was described as “historic.”
The approval of the Medicaid rate increases aligns with the legislature’s decision and contradicts an earlier suggestion to reduce the overall rate increases. The Legislative Fiscal Division‘s analysis estimated that the combined state and federal funds would increase by $339.4 million during fiscal years 2024 and 2025. This move has been welcomed by advocates for behavioral health providers and other affected services, who believe that the increased reimbursements will greatly benefit Montana’s mental health system.
During the 2023 Legislature, the debate revolved around the extent to which Medicaid reimbursements for certain types of providers should be increased
Responding to a commissioned study that revealed underpayment of behavioral health, developmental disabilities, senior, and long-term care providers, both Republicans and Democrats aimed to address this gap, albeit with different perspectives. While Democrats and providers sought to meet the benchmarks outlined in the study, some Republicans expressed concerns about injecting a significant amount of funds into the healthcare industry, fearing potential repercussions during future budget shortfalls.
Healthcare providers, who rely heavily on Medicaid patients, emphasized the importance of fully funding the rates identified in the study to prevent further closures of healthcare facilities. Insufficient Medicaid reimbursement rates were cited as a leading cause of closures in nursing homes, group homes, and behavioral health services. Eventually, bipartisan support for funding rate increases prevailed, aligning the rates with those outlined in the contracted study. Providers expecting the largest rate increases expressed relief and believed that the governor’s approval would alleviate financial strain in the years ahead.